Attitude and Perception Among Emergency Department Healthcare Workers on Organ Donation: A Multicenter Before and After Study
Richard Henry S. Santos, Marilyn B. Puyot, Pauline F. Convocar, Kayleen Bautista, Faith Joan Mesa-Gaerlan, Marjorie Cruz, Sheri Anne Cabañes, Ma. Kristella Gonzales, Amerigo Bautista, Camille Sta. Cruz, Solita de Jesus
Apr 2023 DOI 10.35460/2546-1621.2023-0039
Introduction
Organ transplantation is the most important treatment option for final-stage organ disease and organ failure. The recent decades saw significant advances in the field of organ transplantation resulting in higher success rates and remarkable improvement in the quality of life of patients with terminal organ failure.[1] Under the Organ Donation Act (RA 7170) of 1991, the Philippines has successfully performed kidney, liver, pancreas, bone marrow, and islet cell transplants as well as double transplants like liver and kidney or pancreas and kidney. Currently, there are 28 Department of Health (DOH) accredited transplant facilities in the country. Despite these measures and excellent outcomes of transplant procedures, the number of organ donors to meet the increasing demand in the country continues to lag behind with donation rate remaining low. As per the 2019 data from the International Registry in Organ Donation and Transplantation (IRODAT), the rate of deceased organ donation in western countries such as the United States was 36.88 patients per million population (ppmp) and 48.9 ppmp in Spain, while the Philippines only had a rate of 0.087 ppmp.[4] To address this shortage, there is a need to look into the process of organ donation and identify areas where interventions can be directed for it to be successful.
The complex process of organ donation begins with the most important step, the identification of potential donors – often brain-dead patients or those with irreversible cerebral damage. This crucial stage is the responsibility of healthcare professionals, especially those working in critical areas of the hospital.[5] In several studies, one potential barrier identified is the HCWs perception and attitude toward organ donation. The healthcare professional is placed in a strategic position between the organ donor and transplant recipient playing a pivotal role in the successful donation process. It has been suggested that the perception and attitudes of these professionals have a positive correlation with public’ awareness and willingness to donate while any negative stance may adversely influence the families of potential donors. There is also a high likelihood that a healthcare professional will request an organ donation from a family if they are willing to donate their organs. In contrast, it is estimated that as much as 20% of potential donors are lost secondary to the negative attitude of HCWs.[6,7]
Outside the intensive care unit, the emergency department (ED) was identified in several foreign studies to be a significant source of successful organ donation. Moreover, potential donors referred from the ED were found to be associated with a higher likelihood of success compared to those from other units in the hospital.[8] In a systematic review performed by McCallum, et al, they concluded that 4% - 50% of successful organ donations came from the ED after neurologic determination of death and 3.6% - 8.9% after circulatory determination of death. On the other hand, as much as 84% and 46.2% of missed neurologic determination of death and missed circulatory determination of death, respectively, were also documented following deaths in the ED. Many of these cases often go unrecognized because of poor awareness of staff, physicians and nurses alike.[9] For this reason, the ED healthcare personnel must be targeted for interventions that would increase actual donors while decreasing missed donors.
Analyses of health professional attitudes and perceptions on organ donation have been performed in other countries but a lot about this topic is not known in the Philippines, especially for personnel working in the acute and emergency care setting. There are even lesser studies incorporating an intervention to improve these factors. In this action research project, investigators will compare the attitude and perception of ED HCWs on organ donation before and after an awareness event on organ donation. The main objective of this action research project is to determine the effectiveness of an awareness event to improve the attitude and perception of organ donation of ED HCWs in selected institutions in Metro Manila, Philippines.
Methodology
Clearance and approval from the institutional research ethics committees were sought prior to conduct of the study. All physicians and nurses of participating institutions employed in the ED for more than six months were included in the study. Out of the estimated 287 ED personnel, 125 consented to participate in the study. This represents 43% of the target population.
In April 2021, an awareness event was conducted for ED healthcare professionals in three tertiary hospitals in Metro Manila, Philippines which included interactive sessions on organ donation. The educational part included materials that highlighted global and local statistics on organ donations, types of organ donations, an overview of the process, as well as legal and ethical issues related to organ donations.
All participants were asked to answer the same online pre-structured questions to determine their attitude and perception regarding organ donation immediately before and after the online awareness event. The questionnaire used in this study was prepared from a previous study conducted by the Organ Donation Innovative Strategies for South East Asia (ODISSeA).[10] The survey was composed of two parts; part 1 addressed the socio-demographic information of participants and part 2 addressed information regarding attitude and perception towards organ donation.
The data collected was analyzed statistically using proportions and frequencies and the difference between the two scores was analyzed using paired t-tests to find changes which were observed before and after providing the awareness event intervention.
Results
One hundred twenty-five ED healthcare professionals including nurses, residents and consultants of Pasig City General Hospital, Philippine General Hospital and Manila Doctors Hospital voluntarily participated in this study. The demographics of participants are shown in Table 1. Most respondents were female (60%), aged 25-40 years old (77.60%), single (80%), not dependent (80.8%) and had no known comorbidities (70.4%). The most common comorbidities of respondents were asthma, hypertension and diabetes mellitus. A majority of respondents were Emergency Medicine Residents (43.2%), never had any form of training in organ donation (96.80%) and were in clinical practice for less than 5 years (52%).
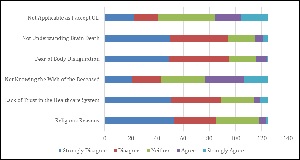
Attitude and perception of organ donation are shown in Table 2 and Figure 1 depicting demographics of HCWs on their attitude regarding willingness to donate their organs after death before the awareness event. Before the awareness event, majority of the participants already had a positive perception of organ donation at 71.2%, and that the respondents’ demographic profiles did not show any association with the attitude on willingness to donate after death. Female (59.6%), age 25 – 40 years old (74.2%), single (79.8%), resident physicians (44.9%), with less than 5 years of experience (50.6%) and no known comorbidities (70.8%) and dependents (79.8%) were more likely to donate their organs after death. Twenty-eight (22.4%) of the respondents were neutral in their willingness to donate organs after death before the awareness event. Only a small number (N – 8, 6.4%) of respondents were not willing to donate their organs after death. The characteristics of respondents who were less likely to donate their organs after death before the awareness event was single, aged 25-40 years old, and residents with less than 5 years of practice. Figure 1 shows that respondents perceive organ donation as equal to solidarity, usefulness, generosity and respect. Most respondents also strongly disagree that organ donation is equal to health care failure, body mutilation, pain and mistrust.
Table 1. Demographics of Participant
|
VARIABLE |
FREQUENCY N = 125 |
PERCENT |
|
|
AGE |
|||
|
<25 |
8 |
6.40% |
|
|
25-40 |
97 |
77.60% |
|
|
40-60 |
19 |
15.20% |
|
|
>60 |
1 |
0.80% |
|
|
SEX |
|||
|
MALE |
50 |
40.00% |
|
|
FEMALE |
75 |
60.00% |
|
|
CIVIL STATUS |
|||
|
SINGLE |
99 |
79.20% |
|
|
MARRIED |
25 |
20.00% |
|
|
SEPARATED/ WIDOWED |
1 |
0.80% |
|
|
NO. OF CHILDREN |
|||
|
NONE |
101 |
80.80% |
|
|
1 |
11 |
8.80% |
|
|
2 |
9 |
7.20% |
|
|
> 2 |
4 |
3.20% |
|
|
PROFESSION |
|||
|
CONSULTANT |
26 |
20.80% |
|
|
RESIDENT |
54 |
43.20% |
|
|
NURSE |
45 |
36.00% |
|
|
YEARS OF PRACTICE |
|||
|
<5 YRS |
65 |
52.00% |
|
|
5-10 YRS |
30 |
24.00% |
|
|
>10 YRS |
30 |
24.00% |
|
|
PRESENCE OF COMORBIDITIES |
|||
|
NONE |
95 |
76.00% |
|
|
YES |
30 |
24.00% |
|
|
TRAINING IN ORGAN DONATION |
|||
|
YES |
4 |
3.20% |
|
|
NO |
121 |
96.80% |
|
Table 2. Pre-Awareness Event Intervention Attitude among Healthcare Workers on their Willingness to Donate their Organs after Death
|
|
WILLING TO DONATE |
NEUTRAL |
WILL NOT DONATE |
|
NUMBER |
89 (71.2%) |
28 (22.4%) |
8 (6.4%) |
|
SEX (P value 0.758) |
|||
|
FEMALE |
53 (59.6%) |
18 (64.3%) |
4 (50%) |
|
MALE |
36 (40.4%) |
10 (35.7%) |
4 (50%) |
|
CIVIL STATUS (P value 0.948) |
|||
|
SINGLE |
71 (79.8%) |
22 (78.6%) |
7 (87.5%) |
|
MARRIED |
17 (19.1%) |
6 (21.4%) |
1 (12.5%) |
|
SEPARATED |
1 (1.1) |
0 |
0 |
|
NO. OF CHILDREN (P value 0.850) |
|||
|
WITH DEPENDENTS |
18 (20%2) |
5 (17.9%) |
1 (12.5%) |
|
NONE |
71 (79.8%) |
23 (82.1%) |
7 (87.5%) |
|
AGE GROUP (P value 0.235) |
|||
|
< 25 |
6 (6.7%) |
2 (7.2%) |
0 |
|
25 – 40 |
66 (74.2%) |
23 (82.1%) |
8 (100%) |
|
41-60 |
17 (19.1%) |
2 (7.2%) |
0 |
|
> 60 |
0 |
1 (3.5%) |
0 |
|
PROFESSION (P value 0.55) |
|||
|
NURSES |
26 (29.2%) |
16 (57.1%) |
4 (50.0%) |
|
RESIDENTS |
40 (44.9%) |
10 (35.7%) |
3 (37.5%) |
|
CONSULTANTS |
23(24.9%) |
2 (7.2%) |
1(12.5%) |
|
YEARS OF PRACTICE (P value 0.914) |
|||
|
< 5 YEARS |
45 (50.6%) |
17 (60.7%) |
4 (50.0%) |
|
5 - 10 YEARS |
22 (24.7%) |
5 (17.9%) |
2 (25.0%) |
|
> 10 YEARS |
22 (24.7%) |
6(21.4%) |
2 (25.0%) |
|
PRESENCE OF COMORBIDITIES (P value 0.878) |
|||
|
NONE |
63 (70.8%) |
20 (71.4%) |
5 (62.5%) |
|
WITH COMORBIDITIES |
26 (29.2%) |
8 (28.6%) |
3 (37.5%) |
Figure 1. Pre-Awareness Event Intervention Perception among Healthcare Workers on Organ Donation

Association of demographics and attitudes of HCWs on organ donation before the awareness event are shown in Table 3 and Figure 2. Most of the respondents are willing to donate their organs at the time of their death and are willing to support organ donation. Half of the respondents were uncertain about donating their relatives’ organs but some are willing to donate their relatives’ organs at the time of their death. The participants were less proactive in proposing organ donation in their clinical environment.
Table 3. Association of Demographic Factors with Attitudes towards Organ Donation
|
I would donate my organs after death. |
I would donate the organs of my relatives after death |
If I am personally against organ donation, I would not propose it in my clinical environment as a healthcare professional. |
In case myself or one of my relatives are diagnosed with end-stage organ failure I will support organ transplantation. |
||
|
`Sex |
Male |
4.04 |
3.44 |
2.36 |
4.12 |
| Female |
3.96 |
3.25 |
2.43 |
4.05 |
|
| P value |
0.307 |
0.458 |
0.641 |
0.527 |
|
|
|
|||||
|
Civil Status |
Married |
4.08 |
3.25 |
2.36 |
4.08 |
| Separated or Widowed |
5.00 |
4.00 |
1.00 |
5.00 |
|
| Single |
3.96 |
3.34 |
2.42 |
4.07 |
|
| P value |
0.529 |
0.768 |
0.518 |
0.524 |
|
|
|
|
|
|
||
|
Age Group |
< 25 y |
4.00 |
3.00 |
3.13 |
3.88 |
| 25 – 40 y |
3.91 |
3.33 |
2.35 |
4.10 |
|
| 41 – 60 y |
4.47 |
3.47 |
2.37 |
4.11 |
|
| > 60 y |
3.00 |
3.00 |
2.00 |
3.00 |
|
| P value |
0.113 |
0.757 |
0.388 |
.0500 |
|
|
|
|
|
|
|
|
|
Profession |
Consultant |
4.38 |
3.42 |
2.31 |
4.19 |
| Resident |
4.08 |
3.58 |
2.23 |
4.30 |
|
| Nurse |
3.67 |
2.98 |
2.65 |
3.76 |
|
| P value |
0.01 |
0.01 |
0.210 |
0.00 |
|
|
|
|||||
|
Length of Service |
< 5 y |
3.89 |
3.32 |
2.42 |
3.97 |
| 5 – 10 y |
4.07 |
3.52 |
2.14 |
4.41 |
|
| > 10 y |
4.13 |
3.17 |
2.60 |
4.00 |
|
| P value |
0.507 |
0.453 |
0.347 |
0.38 |
|
Figure 2. Pre-Awareness Event Intervention Attitudes among Healthcare Workers on Organ Donation

The possible reasons for non-acceptance of organ donation were shown in Figure 3. Nearly every healthcare provider believes that organ donation must not be hindered by religious beliefs, lack of trust in the healthcare system, lack of understanding of brain death and fear of body disfiguration. The possible cause of organ donation denial among participants is due to not knowing the wish of the deceased.
Figure 3. Possible Reasons for Non-Acceptance of Organ Donation

The perception of healthcare provider confidence level regarding organ donation is shown in Table 4. The participants agree that undergoing proper training would make them confident to talk about organ donation. To further boost their confidence in discussing organ donation, they believe that organ donation must be supported by having a legal framework and part of an end-of-life care program. Most of the participants (41.6%) were neutral with regard to ICU admission of patients with devastating injuries for the sole purpose of organ donation. Also, a large number of participants (61.6%) agreed to employ the same resources to maintain a potential brain-dead donor as in any other critical patient.
Table 4. Pre-Awareness Event Intervention Perception of One’s Confidence Regarding Organ Donation
|
1 STRONGLY DISAGREE |
2 DISAGREE |
3 NEITHER |
4 AGREE |
5 STRONGLY AGREE |
|
| I am confident to talk about organ donation in my clinical environment if I am correctly trained on this matter. |
2 (1.6%) |
9 (7.2%) |
9 (7.2%) |
42 (33.6%) |
63 (50.4%) |
| I am confident to talk about organ donation in my clinical environment if organ donation is supported by a legal framework. |
0 |
7 (5.6%) |
13 (10.4%) |
42 (33.6%)
|
63 (50.4%) |
| Organ donation should be part of the end of life care. |
0 |
3 (2.4%) |
30 (24.0%) |
33 (26.4%) |
59 (47.2%) |
| I feel comfortable talking to the relatives about end-of-life care, brain death or organ donation according to my position in the hospital. |
1 (8%) |
19 (15.2%) |
1 (32.8%) |
40 (32.0%) |
24 (19.2%) |
| I agree with the admission to the Intensive Care Unit of patients with devastating injuries in whom the treatment has been deemed futile, for the solely reason of facilitating organ and tissue donation. |
7 (5.6%) |
19 (15.2%) |
52 (41.6%) |
33 (26.4%) |
14 (11. 2%) |
| I consider appropriate to employ the same resources to maintain a potential brain-dead donor as in any other critical patient |
2 (1.6%) |
7 (5.6%) |
39 (31.2%) |
50 (40.0%) |
27 (21.6%) |
There was varied response among respondents on when was the appropriate moment to talk about organ donation as shown in Figure 4. Most of the respondents agreed it was appropriate to talk about organ donation when death of the patient was predictable (54.4%) and after the patient’s death.
Figure 4. Distribution of Responses Regarding Most Appropriate Moment to Discuss Organ Donation

Following the online virtual awareness event, there was a higher positive perception and a lower negative perception of participants regarding organ donation. However, only the change in the perception relating to solidarity, generosity and respect was statistically significant.
The attitudes of HCWs regarding their willingness to donate before and after the awareness event are shown in Table 4. After the awareness event, a significant increase in the number of respondents (p-value <0.5%) was noted willing to donate their organs after death. There is a decline in respondents who are neutral and not willing to donate their organs after death. There is also an increase in the number of participants willing to donate organs of their relatives after their death after the awareness event.
Table 4. Attitudes of the Healthcare Workers regarding their Willingness to Donate Before and After the Awareness Event
|
|
BEFORE INTERVENTION |
AFTER INTERVENTION |
P-VALUE |
|
WILLINGNESS TO DONATE OWN ORGANS |
|||
|
WILLING TO DONATE |
89 (71.2%) |
99 (79.2%) |
0 |
|
NEUTRAL |
36 (40.4%) |
10 (35.7%) |
|
|
NOT WILLING TO DONATE |
28 (22.4%) |
23 (18.4%) |
|
|
WILLINGNESS TO DONATE RELATIVES’ ORGANS |
|||
|
WILLING TO DONATE |
49 (39.2%) |
58 (46.4%) |
0.03 |
|
NEUTRAL |
57 (45.6%) |
55 (44%) |
|
|
NOT WILLING TO DONATE |
19 (15.2%) |
12 ((9.6%) |
|
The possible reasons for non-acceptance of organ donation were shown in Figure 5. Nearly every one of the healthcare providers believes that organ donation must not be hindered by religious beliefs, lack of trust in the healthcare system, lack of understanding of brain death and fear of body disfiguration. The possible cause of organ donation denial among participants is due to not knowing the wish of the deceased.
Figure 5. Possible Reasons for Non-Acceptance of Organ Donation

Table 6. Comparison of Pre and Post-Awareness Event Intervention Online Survey Answers of Participant
|
Pre-test |
Post-test |
P-value |
Interpretation |
|||
|
Mean |
SD |
Mean |
SD |
|||
| 1. In my personal opinion, organ donation is equal to … | ||||||
| SOLIDARITY |
4.38 |
.737 |
4.63 |
.501 |
0.00 |
Significant |
| USEFULNESS |
4.54 |
.746 |
4.62 |
.656 |
0.33 |
Not Significant |
| GENEROSITY |
4.49 |
.769 |
4.66 |
.567 |
0.01 |
Significant |
| RESPECT |
4.41 |
.753 |
4.59 |
.610 |
0.00 |
Significant |
| HEALTHCARE FAILURE |
2.01 |
1.13 |
2.01 |
1.13 |
1.00 |
Not Significant |
| MUTILATION |
2.02 |
1.27 |
1.86 |
1.02 |
0.08 |
Not Significant |
| PAIN |
1.83 |
1.13 |
1.82 |
1.03 |
0.93 |
Not Significant |
| MISTRUST |
1.96 |
1.15 |
1.90 |
1.09 |
0.50 |
Not Significant |
|
|
|
|
|
|
|
|
| 2. I would donate my organs after death. |
3.99 |
1.01 |
4.26 |
.870 |
0.00 |
Significant |
| 3. I would donate the organs of my relatives after death. |
3.33 |
1.07 |
3.51 |
1.01 |
0.03 |
Significant |
| 5. If I am personally against organ donation, I would not propose it in my clinical environment as a healthcare professional. |
2.40 |
1.23 |
2.70 |
1.46 |
0.07 |
Not Significant |
| 13. In case myself or one of my relatives are diagnosed with end-stage organ failure I support organ transplantation. |
4.08 |
.809 |
4.27 |
.700 |
0.01 |
Significant |
|
|
|
|
|
|
|
|
| 6. I am confident to talk about organ donation in my clinical environment if I am correctly trained on this matter. |
4.24 |
.979 |
4.28 |
.912 |
0.58 |
Not Significant |
| 7. I am confident to talk about organ donation in my clinical environment if organ donation is supported by a legal framework. |
4.29 |
.869 |
4.33 |
.860 |
0.65 |
Not Significant |
| 9. I feel comfortable talking to the relatives about end of life care, brain death or organ donation according to my position in the hospital. |
4.18 |
.883 |
4.32 |
.790 |
0.03 |
Significant |
| 11. I agree with the admission to the Intensive Care Unit of patients with devastating injuries in whom the treatment has been deemed futile, for the sole reason of facilitating organ and tissue donation. |
3.22 |
1.02 |
3.74 |
1.11 |
0.00 |
Significant |
| 12. I consider appropriate to employ the same resources to maintain a potential brain-dead donor as in any other critical patient |
3.74 |
.914 |
4.00 |
.911 |
0.00 |
Significant |
|
|
|
|
|
|
|
|
| 10. APPROPRIATE TIME TO TALK ABOUT ORGAN DONATION | ||||||
| Anytime |
2.88 |
1.11 |
2.90 |
1.25 |
.83 |
Not Significant |
|
When the death of the patient is predictable |
3.70 |
.950 |
3.83 |
.973 |
.17 |
Not Significant |
|
After the patient’s death |
2.95 |
1.08 |
3.26 |
1.17 |
.00 |
Significant |
| Never |
1.94 |
.859 |
1.70 |
.863 |
.00 |
Significant |
|
|
|
|
|
|
|
|
| 4. ACCEPTANCE OF ORGAN DONATION | ||||||
| Religious Beliefs |
1.97 |
1.00 |
2.00 |
.976 |
.71 |
Not Significant |
|
Lack of trust in the healthcare system |
2.02 |
1.10 |
1.96 |
.976 |
.51 |
Not Significant |
|
Not knowing the wish of the deceased |
3.02 |
1.30 |
3.26 |
1.50 |
.10 |
Not Significant |
|
Fear of body disfiguration |
1.93 |
.943 |
2.06 |
1.13 |
.13 |
Not Significant |
|
Not understanding brain death |
1.96 |
1.07 |
1.97 |
1.07 |
.93 |
Not Significant |
|
Not applicable as I accept organ donation |
2.99 |
1.30 |
3.21 |
1.47 |
.17 |
Not Significant |
Discussion
This study documented the attitude and perception of emergency department healthcare workers (ED HCWs) on organ donation involving three tertiary hospitals in the Philippines, namely Philippine General Hospital, Manila Doctors Hospital and Pasig City General Hospital; all are level 3 hospitals with emergency medicine residency training programs. The research project was conducted without taking into consideration the participant’s present knowledge or experience in organ donation. As per literature review on published studies using scholarly search engines, this may be the first and only study done in the Philippines to document the attitude and perception of ED HCWs on organ donation and the impact of an awareness event intervention. There is an identified research need on this aspect which this study attempts to address as the ED HCWs are relatively underrecognized in their important role in the organ donation process. This study revealed that ED nurses and doctors are generally supportive and hold positive perceptions and attitudes towards organ donation. This is important in organ donation process because it influences their professional behavior in requesting organ donation from families who lost their loved ones, thereby increasing the chances of a successful organ donation outcome.[11]
This study revealed that most of the emergency HCWs were generally supportive and held a positive perception and attitude towards organ donation even before the awareness event. It is further fortified by the awareness event. The stronger willingness to donate may be associated with higher education level and profession of our participants as seen in the study of Wei, et al.[13] Strong willingness to donate is important in the organ donation process because it influences their professional behavior in requesting organ donation from families who lost their loved ones, thereby increasing chances of a successful outcome.[11] In the current study, physicians have a higher and more significant level of willingness to donate compared to nurses. This finding is similar to findings of a literature review on healthcare personnel views on organ donation and transplantation and with physicians having a more positive attitude towards organ donation than other clinical staff[12,14], although reasons for the above findings have not been the subject of studies.
The study revealed that the ED HCWs are less proactive in promoting organ donation in their clinical environment and they agree that undergoing proper training would make them confident to talk about organ donation. To further boost their confidence in discussing organ donation, they believe that organ donation must be supported by having a legal framework and part of an end-of-life care program. It is similar to a Polish study, in which physicians from countries with low donation rates were less proactive in promoting organ donation in brain-dead patients. The biggest obstacles indicated by physicians in the Polish study were related to communication with family of the deceased and they expressed the need for standards and training in organ donation. Bøgh, et al. showed a need for training not only in medical issues (potential donor identification), but also in psychological ones (information and support to deceased relatives).[15]
Despite the positive attitude, majority of HCWs seem to be uncomfortable or unwilling to perform tasks important to organ donation such as approaching relatives, and management of the deceased organ donor. It is imperative that there should be an improvement in overall confidence in the skill of communicating organ donation, and deceased organ donor management among the ED HCWs and not just limited to targeting an improvement in attitude. The value of this need is on the premise that detection of potential organ donors starts in the ED and serves as the trigger to initiate entire organ donation process. In a study by Marloes, et al, a multidisciplinary approach for potential organ donors in the ED showed that collaboration between the ED and other specialty (Neurology, Neurosurgery and ICU) has led to better results for organ donation and few missed donors than starting a referral for organ donation once the patient is admitted to the ICU.[13] This supports the importance of increasing awareness and improving attitude among the ED staff.
The majority of ED staff holds very positive personal attitudes toward organ donation, but all of them were not able to formally translate this to signing their organ donation cards and registering this desire to donate in a formal registry of would-be donors in the Philippines. The inaction may be due to an access block as to the lack of a formal system for the said registry. The desire to donate organs after death in the Philippines is expressed only by signing the organ donor card distributed by advocacy groups such as the National Kidney Transplant Institute - Human Organ Preservation Effort (NKTI-HOPE) or signifying the desire to donate by ticking the option at the back of the Philippines Driver’s License. Discussing this decision with their family is explicit only when the family member co-signs the Organ Donation Card. The results of this study also reflect the situation of the general Filipino population regarding their decision to donate their organs after death.
After the awareness event on organ donation, a significant increase in the number of ED HCWs willing to donate their organs after death was noted. Targeting the awareness event intervention to the population (22.4%) of those ED HCWs still undecided about their decision to donate their organs after death may be strategic. The demographic profile of those hesitant was relatively younger at 25-40 years old with less than 5 years of experience in the ED. Half of the respondents also reported and reflected on their uncertainty about donating their relative’s organs after death, which may again be a strategic focus for intervention. The impact of a single intervention such as the awareness event may be further amplified with long-term interventions such as the integration of a formal training program on organ donation targeted to the ED HCWs.
In an Australian study, evidence suggests that attitudes are strongly affected by education. Therefore, education addressing these issues directed to HCWs may aid in removing concerns and improving positive attitudes toward organ donation.[15] The authors recommend that organ donation must be integrated into the curriculum of emergency medicine and nursing training to improve the Philippines’ organ donation program. Sustainable and strategic interventions targeting specific demographic profiles identified in this study may be impactful.
Awareness events as interventions may be considered effective tools to improve attitudes and perceptions of organ donation. Reported willingness to donate may be strengthened with the actual signing of the ED HCWs signing of their organ donation cards or their next-of-kin's. Opportunities for awareness events may present themselves in several forms in health facilities as in orientation and training of newly-hired or appointed personnel including the ED rotators among many other opportunities.
To improve the organ donation program in the Philippines, further studies may need to be sought to consider the value/effect of other complementary interventions as having dedicated organ donation coordinators and clinicians responsible for recognizing and referring potential donors from the ED as well as introducing organ donation to the next of kin or decision-maker. Policy gaps and collaboration opportunities also need to be considered.
Conclusion
This study aimed to examine the effects of an awareness event intervention on ED staff attitudes and perceptions regarding organ donation and transplantation regardless of their present knowledge or experience on the topic. The results of this study revealed that majority of respondents had improved attitudes and perceptions regarding organ donation and transplantation after the awareness event intervention. The emergency HCWs were found to have a positive attitude regarding the organ donation process and that their attitude would be influenced by conducting awareness events, such as the one conducted in this study, to increase the rate of deceased organ donation. This study suggests the need for further research with a large sample and beyond the ED population. Future research should also focus on continuous educational programs that are needed to increase awareness about organ transplantation in various groups in our country.
ACKNOWLEDGMENT
The authors would like to express their gratitude to the Donor and Transplantation Institute (Barcelona, Spain) and Organ Donation Innovative Strategies for Southeast Asia (ODISSeA) for their support in the conduct of this on-the-job research project.
- Grinyo JM. Why is organ transplantation clinically important? Cold Spring Harb Perspect Med. 2013 Jun;3(6):a014985.
- Philippines. An act (No. 7170) authorizing the legacy or donation of all or part of a human body after death for specified purposes. Dated 7 January 1992 (The Organ Donation Act of 1991). (Official Gazette, 24 February 1992, Vol. 88, No. 8, pp. 965-971). Int Dig Health Legis. 1992;43(4). PMID: 11659648.
- Chan-On C, Sarwal MM. A comprehensive analysis of the current status and unmet needs in kidney transplantation in Southeast Asia. Front Med (Lausanne) [Internet]. 2017;4:84. Available from: http://dx.doi.org/10.3389/fmed.2017.00084
- International Registry in Organ Donation and Transplantation (IRODaT) Newsletter March 2020. Retrieved on March 15, 2020. Available at: http://www.irodat.org/img/database/
- Girlanda R. Deceased organ donation for transplantation: Challenges and opportunities. World J Transplant [Internet]. 2016;6(3):451–9. Available from: http://dx.doi.org/10.5500/wjt.v6.i3.451
- Ríos A, López-Navas A, Ayala-García MA, Sebastián MJ, Abdo-Cuza A, Alán J, et al. Estudio multicéntrico hispano-latinoamericano de actitud hacia la donación de órganos entre profesionales de centros sanitarios hospitalarios. Cir Esp [Internet]. 2014;92(6):393–403. Available from: http://dx.doi.org/10.1016/j.ciresp.2013.12.017
- Hu D, Huang H. Knowledge, attitudes, and willingness toward organ donation among health professionals in China. Transplantation [Internet]. 2015;99(7):1379–85. Available from: http://dx.doi.org/10.1097/TP.0000000000000798
- Michael GE, O’Connor RE. The importance of emergency medicine in organ donation: successful donation is more likely when potential donors are referred from the emergency department. Acad Emerg Med [Internet]. 2009;16(9):850–8. Available from: http://dx.doi.org/10.1111/j.1553-2712.2009.00472.x
- McCallum J, Ellis B, Dhanani S, Stiell IG. Solid organ donation from the emergency department - A systematic review. CJEM [Internet]. 2019;21(5):626–37. Available from: http://dx.doi.org/10.1017/cem.2019.365
- ODISSeA project – diagnosis study report. February 2019 [Internet]. Odisseaproject.eu. [cited 2023 Apr 11]. Available from: https://odisseaproject.eu/odissea-project-diagnosis-study-report-february-2019
- Marck CL. Assessing barriers to the involvement of emergency departments in organ donation. Transplantation. 2012;94(10S):147.
- Mercado-Martinez FJ, Padilla-Altamira C, Diaz-Medina B, Sanchez-Pimita C. Views of Healthcare Personnel on Organ Donation and Transplantation: A Literature Review. Text Context Nursing, Florianopolis. Abr-June 2015 24(2):574–83.
- Bch B, Ong JS, Bch B, Foong JW, Bch B, Hossain MM, et al. Knowledge and attitudes of healthcare professionals and the impact on willingness to donate organs: a tertiary hospital survey. Singapore Med J. 2020;61(3):154–61.
- Kosieradzki M, Jakubowska-Winecka A, Feliksiak M, Kawalec I, Zawilinska E, Danielewicz R, et al. Attitude of healthcare professionals: a major limiting factor in organ donation from brain-dead donors. J Transplant [Internet]. 2014;2014:296912. Available from: http://dx.doi.org/10.1155/2014/296912
- Marck CH, Weiland TJ, Neate SL, Hickey BB, Jelinek GA. Personal attitudes and beliefs regarding organ and tissue donation: a cross-sectional survey of Australian emergency department clinicians. Prog Transplant [Internet]. 2012;22(3):317–22. Available from: http://dx.doi.org/10.7182/pit2012311
![]() Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0
International License, which permits use, share — copy and redistribute the material in any medium or format,
adapt — remix, transform, and build upon the material, as long as you give appropriate credit,
provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner,
but not in any way that suggests the licensor endorses you or your use. You may not use the material for
commercial purposes. If you remix, transform, or build upon the material, you must distribute your
contributions under the same license as the original. You may not apply legal terms or technological
measures that legally restrict others from doing anything the license permits. The images or other
third party material in this article are included in the article’s Creative Commons license, unless indicated
otherwise in a credit line to the material. If material is not included in the article’s Creative Commons
license and your intended use is not permitted by statutory regulation or exceeds the permitted use,
you will need to obtain permission directly from the copyright holder. To view a copy of this license,
visit https://creativecommons.org/licenses/by-nc-sa/4.0/.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0
International License, which permits use, share — copy and redistribute the material in any medium or format,
adapt — remix, transform, and build upon the material, as long as you give appropriate credit,
provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner,
but not in any way that suggests the licensor endorses you or your use. You may not use the material for
commercial purposes. If you remix, transform, or build upon the material, you must distribute your
contributions under the same license as the original. You may not apply legal terms or technological
measures that legally restrict others from doing anything the license permits. The images or other
third party material in this article are included in the article’s Creative Commons license, unless indicated
otherwise in a credit line to the material. If material is not included in the article’s Creative Commons
license and your intended use is not permitted by statutory regulation or exceeds the permitted use,
you will need to obtain permission directly from the copyright holder. To view a copy of this license,
visit https://creativecommons.org/licenses/by-nc-sa/4.0/.
